Published: 29 December 2025
Preoperative Assessment: Setting the Scene and Identifying the Risks
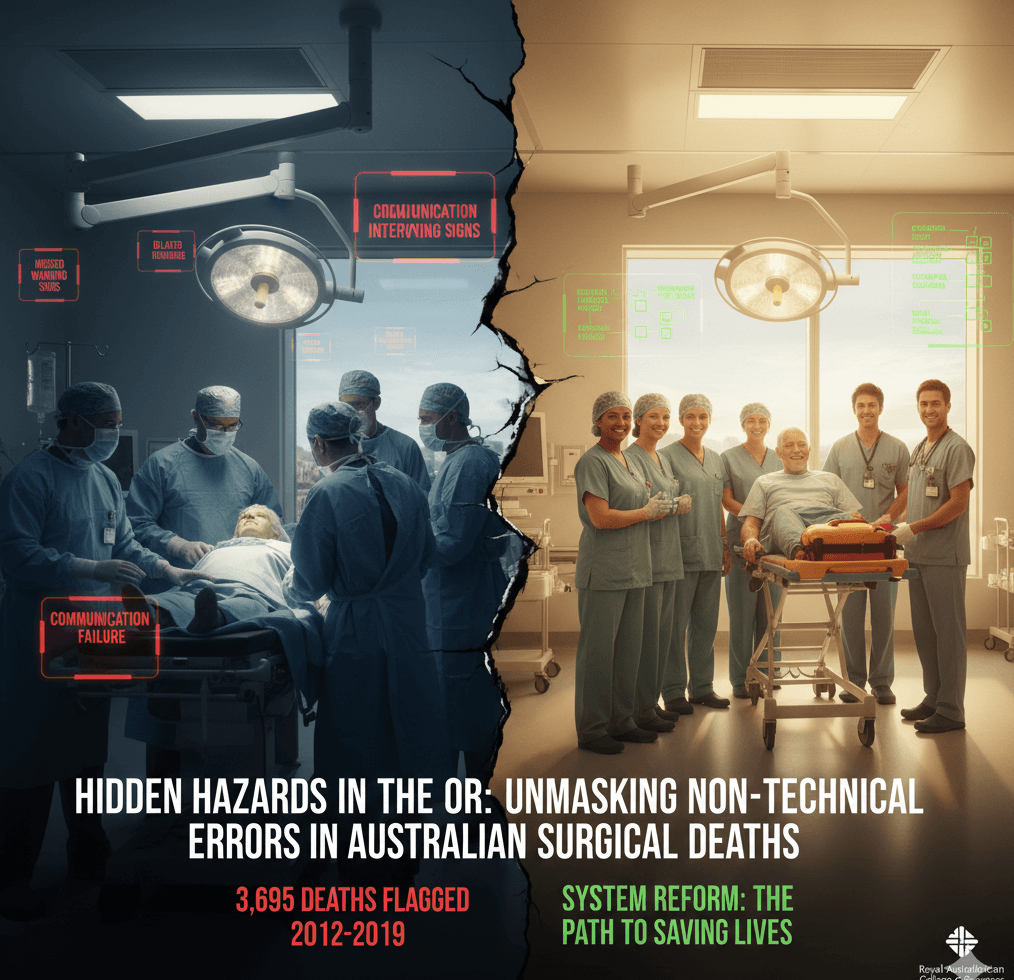
Imagine a patient in their seventies, rushed to hospital with acute abdominal pain. During an emergency transfer between facilities, critical warning signs are missed due to a breakdown in communication between teams. A decision to delay intervention proves fatal, turning a potentially survivable condition into tragedy. This anonymised case, drawn from audited surgical mortality data, is not isolated—it exemplifies the human cost of non-technical errors that plague Australian operating rooms.
A landmark peer-reviewed study by the Australian and New Zealand Audit of Surgical Mortality (ANZASM), published in the Medical Journal of Australia, analysed 30,971 deaths related to surgical care across Australia from 2012 to 2019. Of these, 3,695 cases were flagged for adverse events or areas of concern, with the analysis narrowing to 3,422 deaths in five major specialties: general surgery, cardiothoracic surgery, orthopaedic surgery, vascular surgery, and neurosurgery. Conducted by researchers at the University of Adelaide and supported by the Royal Australasian College of Surgeons (RACS), the study excluded data from New South Wales due to jurisdictional differences, highlighting a need for more comprehensive national coverage.
In the broader context, these non-technical errors—such as poor decision-making, lapses in situational awareness, and communication failures—act as a ‘silent killer’ in surgical settings. Unlike technical mishaps with scalpels or instruments, these stem from human factors that persist despite rigorous audits and safety protocols, underscoring systemic vulnerabilities in Australia’s healthcare landscape.
Incision: Cutting into the Data and Key Findings
Delving deeper, the ANZASM study reveals a stark reality: at least 50 per cent of flagged surgical deaths were associated with non-technical errors, with no meaningful decline over the seven-year period—only minor reductions noted in general surgery. This persistence suggests that current auditing processes, while valuable, have not sufficiently addressed these preventable issues.
Breaking it down by specialty paints a nuanced picture:
| Specialty | % of Flagged Deaths with Non-Technical Errors | Dominant Error Types | Key Notes |
| General Surgery | ~68.5% | Situational awareness > Decision-making | Highest volume of errors; persistent high death counts despite slight decline in error-linked cases. |
| Vascular Surgery | ~60-65% | Decision-making > Situational awareness | High risk in emergency admissions. |
| Cardiothoracic | ~64.5% | Decision-making predominant | Communication issues in transfers are prominent. |
| Neurosurgery | ~55-60% | Decision-making focused | Errors are often tied to judgment in complex cases. |
| Orthopaedic | ~52% | Situational awareness dominant | Lower overall but still significant in flagged deaths. |
Variations in the data show that patient-specific factors, such as age or emergency status, played minimal roles in these errors. Instead, about half involved failures in situational awareness and decision-making, particularly during high-stakes scenarios like emergency admissions and inter-hospital transfers where communication often falters.
Exploration: Probing the Causes and Broader Implications
At the root, these errors arise from trainable non-technical skills like leadership, teamwork, and situational judgement, rather than individual incompetence. Data from the Western Australian Audit of Surgical Mortality (WAASM) reinforces this, with many clinical management issues linked to communication and leadership rather than surgical procedures. Moreover, surgical deaths in Australia have risen since 2020, reversing earlier downward trends, largely due to non-operative cases and overload in general surgery.
Diverse perspectives enrich the discussion. News outlets like 7News Sydney have framed the issue as ‘human errors behind thousands of deaths’, spotlighting missed warnings and delays in care. Online forums, such as Reddit discussions, debate systemic challenges like understaffing versus tools like individual checklists, often referencing World Health Organization safety protocols and aviation-inspired human factors training to advocate for broader reforms.
The implications are profound: elevated error rates signal widespread vulnerabilities in Australia’s healthcare system, where audits alone have failed to drive sufficient change. This ties into related audits, such as WAASM’s emphasis on avoiding non-beneficial surgeries and addressing rising mortality in patients not undergoing operations.
Repair and Reconstruction: Building Solutions from Expert Insights
Experts are vocal on the path forward. Professor Guy Maddern, senior author of the ANZASM study from the University of Adelaide, warns: ‘Inadequate non-technical skills can have fatal consequences, particularly in high-pressure environments such as emergency admissions and inter-hospital transfers where communication breakdowns are common.
Coaching may be one way to deliver this training.’ This contrasts with community sentiments on platforms like Reddit, where users suggest practical measures such as routine debriefs and stricter adherence to checklists to foster a culture of accountability.
Proposed solutions focus on system-wide enhancements rather than isolated fixes, including evidence-based training programmes, coaching, and robust feedback mechanisms. The Australian Commission on Safety and Qualityy in Health Care echoes calls for targeted strategies to combat persistent error rates and further research into effective interventions.
Closure and Recovery: Wrapping Up with a Call to Action
In summary, while surgical deaths in Australia are meticulously audited, non-technical errors remain a preventable threat, potentially contributing to thousands of fatalities each year.
Looking ahead, it’s imperative for healthcare leaders, training institutions, and policymakers to enact reforms, such as nationwide coaching programmes inspired by proven models in aviation. If non-technical skills can save lives in the skies, why not in surgery? With the ANZASM study’s exclusion of NSW data pointing to gaps, ongoing monitoring and national expansion are essential to safeguard future patients